Nicotine: Everything You Need to Know
Nicotine, a substance that has captured the attention of scientists, health professionals, and the public alike, plays a central role in the global tobacco epidemic. This guide aims to provide a thorough understanding of nicotine, its effects on the human body, the risks associated with its use, and effective strategies for overcoming nicotine addiction.
The Origins and Spread of Nicotine Use
Nicotine, named after the tobacco plant from which it’s derived, has a rich and complex history that spans continents and centuries.
From Sacred Plant to Global Commodity
The tobacco plant, native to the Americas, holds deep cultural significance for many indigenous peoples. These communities traditionally used tobacco for medicinal, spiritual, and social purposes. However, the arrival of European colonizers in the 15th and 16th centuries transformed tobacco from a sacred plant into a global commodity.
European traders quickly recognized tobacco’s addictive properties and its potential for profit. They began large-scale cultivation and exportation of tobacco, spreading its use across the globe. This shift marked the beginning of tobacco’s transition from a plant used in ceremonial contexts to a widely consumed recreational substance.
The Rise of the Tobacco Industry
As tobacco use spread, a powerful industry emerged to meet the growing demand. By the 20th century, tobacco companies had become some of the largest and most influential corporations in the world. These companies employed sophisticated marketing strategies to promote their products and expand their customer base.
One particularly controversial aspect of tobacco marketing has been the targeting of specific demographic groups. Research has shown that tobacco companies have disproportionately marketed their products, especially menthol cigarettes, to racial minorities and low-income communities1. This targeted marketing has contributed to significant health disparities among different populations.
The Centers for Disease Control and Prevention (CDC) reports that non-Hispanic Black or African American individuals are more likely to smoke menthol cigarettes than other racial or ethnic groups2. This is particularly concerning because menthol may increase nicotine’s addictiveness, making it harder for users to quit and increasing their risk of tobacco-related diseases.
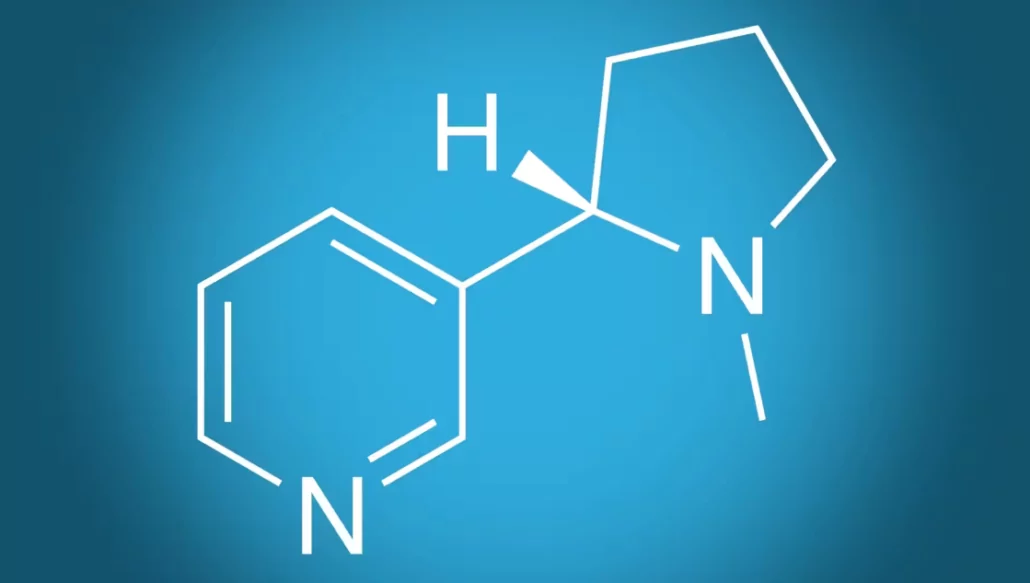
The Science of Nicotine: How It Affects the Brain and Body
To truly understand the impact of nicotine, it’s crucial to explore how this substance interacts with the human body on a molecular level.
Nicotine’s Journey Through the Body
When a person uses a nicotine-containing product, whether it’s a traditional cigarette, an e-cigarette, or another form of tobacco, the nicotine rapidly enters the bloodstream. From there, it travels to the brain in a matter of seconds. This quick action is one of the reasons nicotine is so addictive – it provides almost instant gratification to the user.
Neurochemical Effects
Once in the brain, nicotine triggers a series of chemical reactions that profoundly affect mood, cognition, and behavior:
- Dopamine Release: Nicotine stimulates the release of dopamine, a neurotransmitter associated with pleasure and reward. This flood of dopamine creates a sense of euphoria and reinforces the behavior of nicotine use, contributing to the development of addiction3.
- Endorphin Production: Nicotine also prompts the release of endorphins, the body’s natural painkillers. This leads to feelings of relaxation and reduced stress, which many users find appealing.
- Cognitive Enhancement: In the short term, nicotine can improve attention, memory, and reaction time. These cognitive benefits, however, are typically short-lived and do not outweigh the long-term risks of nicotine use.
- Adrenaline Surge: Nicotine triggers the release of adrenaline, increasing heart rate, blood pressure, and breathing rate. This “fight or flight” response can make the user feel more alert and energized.
Physiological Effects
Nicotine’s impact extends beyond the brain, affecting various bodily systems:
- Cardiovascular System: Nicotine increases heart rate and blood pressure, putting additional strain on the heart. It also promotes the buildup of fatty acids in the arteries, increasing the risk of heart disease and stroke4.
- Respiratory System: While nicotine itself doesn’t cause lung cancer, tobacco smoke contains numerous carcinogens that damage the lungs. Nicotine can also exacerbate respiratory conditions like asthma.
- Digestive System: Nicotine can increase acid production in the stomach, leading to heartburn and potentially contributing to the development of ulcers. It may also reduce appetite, which is why some people gain weight when they quit smoking.
- Endocrine System: Nicotine interferes with the body’s ability to regulate blood sugar, potentially increasing the risk of type 2 diabetes. It can also affect hormone production, impacting everything from mood to reproductive health.
The Addictive Nature of Nicotine
Understanding nicotine addiction requires a closer look at how this substance changes the brain over time.

The Cycle of Addiction
Nicotine addiction develops through a cycle of repeated exposure and withdrawal:
- Initial Use: When a person first uses nicotine, they often experience pleasurable effects due to the release of dopamine and other neurotransmitters.
- Tolerance: With continued use, the brain adapts to the presence of nicotine. This means that more nicotine is needed to achieve the same effects, leading to increased consumption.
- Dependence: As tolerance develops, the brain begins to rely on nicotine to function normally. At this stage, the absence of nicotine leads to withdrawal symptoms.
- Withdrawal and Craving: When a dependent person stops using nicotine, they experience uncomfortable withdrawal symptoms like irritability, anxiety, and strong cravings. These symptoms often drive the person to use nicotine again, perpetuating the cycle of addiction.
Why Nicotine is So Addictive
Several factors contribute to nicotine’s high addictive potential:
- Rapid Action: Nicotine reaches the brain within seconds of inhalation, providing almost instant gratification.
- Frequent Dosing: The short-lived effects of nicotine, combined with the ease of using tobacco products, lead to frequent dosing throughout the day. This repeated exposure strengthens the addictive pathways in the brain.
- Associative Learning: People often use tobacco in specific situations or emotional states. Over time, these situations or emotions can trigger cravings, even in the absence of physical withdrawal.
- Genetic Factors: Research suggests that genetic variations can influence how individuals respond to nicotine, affecting their likelihood of becoming addicted5.
Health Risks Associated with Nicotine Use
While nicotine itself is not carcinogenic, its most common delivery method – smoking – is the leading preventable cause of death worldwide. The health risks associated with nicotine use are numerous and severe:

Cardiovascular Diseases
Nicotine use significantly increases the risk of heart disease, stroke, and peripheral vascular disease. It does this by:
- Increasing heart rate and blood pressure
- Promoting the formation of blood clots
- Contributing to the buildup of plaque in the arteries
- Reducing the amount of oxygen-rich blood flowing to the heart
Respiratory Diseases
While nicotine itself doesn’t cause lung cancer, tobacco smoke contains numerous carcinogens that damage the lungs. Smoking is the leading cause of lung cancer and chronic obstructive pulmonary disease (COPD). Even e-cigarette use has been associated with lung damage, though the long-term effects are still being studied6.
Cancer
Tobacco use is linked to numerous types of cancer, including:
- Lung cancer
- Throat and mouth cancer
- Pancreatic cancer
- Bladder cancer
- Cervical cancer
Reproductive Health
Nicotine can have significant impacts on reproductive health:
- In men, it can lead to reduced sperm count and increased risk of erectile dysfunction.
- In women, it can cause reduced fertility and increased risk of complications during pregnancy.
- Nicotine use during pregnancy can lead to low birth weight, premature birth, and increased risk of birth defects.
Mental Health
While some people use nicotine to manage stress or anxiety, long-term use can actually worsen mental health. Nicotine addiction is associated with increased rates of depression and anxiety7.
The E-Cigarette Debate: A Safer Alternative or a New Threat?
Electronic nicotine delivery systems (ENDS), commonly known as e-cigarettes or vapes, have emerged as a popular alternative to traditional cigarettes. These devices heat a liquid containing nicotine, solvents, and flavorings to produce vapor instead of smoke.

Potential Benefits of E-Cigarettes
Proponents of e-cigarettes argue that they offer several advantages over traditional cigarettes:
- Fewer Harmful Chemicals: E-cigarettes don’t produce tar or carbon monoxide, two of the most harmful elements in tobacco smoke.
- Potential for Harm Reduction: Some studies suggest that e-cigarettes may be less harmful than traditional cigarettes and could potentially help smokers quit8.
- Reduced Secondhand Exposure: The vapor from e-cigarettes contains fewer harmful chemicals than secondhand smoke, potentially reducing risks to bystanders.
Concerns and Risks
However, e-cigarettes are not without risks:
- Unknown Long-Term Effects: E-cigarettes are relatively new, and their long-term health effects are not yet fully understood.
- Youth Appeal: The variety of flavors and sleek designs of e-cigarettes have made them particularly appealing to young people, raising concerns about a new generation becoming addicted to nicotine9.
- Potential Gateway Effect: Some research suggests that e-cigarette use among youth may lead to later use of traditional tobacco products.
- Acute Lung Injury: There have been reports of severe lung injuries associated with vaping, particularly with products containing THC10.
Breaking the Nicotine Habit: Evidence-Based Treatment Options
Overcoming nicotine addiction is challenging but achievable with the right support and treatment. Here are the most effective strategies based on current scientific evidence:

1. Nicotine Replacement Therapy (NRT)
NRT provides controlled doses of nicotine without the harmful chemicals found in tobacco smoke. FDA-approved NRT products include:
- Nicotine patches
- Nicotine gum
- Nicotine lozenges
- Nicotine nasal spray
- Nicotine inhalers
These products can significantly reduce withdrawal symptoms and cravings, making it easier for individuals to quit smoking. Research has shown that NRT can increase the likelihood of successful quitting by 50% to 60%11.
2. Prescription Medications
Several medications have proven effective in treating nicotine dependence:
- Bupropion (Zyban): An antidepressant that reduces cravings and withdrawal symptoms. It works by affecting the brain chemicals involved in nicotine addiction.
- Varenicline (Chantix): This medication partially stimulates nicotine receptors, reducing both cravings and the pleasurable effects of smoking. Studies have shown it to be more effective than bupropion in helping people quit smoking12.
3. Behavioral Therapy and Counseling
Psychological support plays a crucial role in overcoming nicotine addiction. Effective approaches include:
- Cognitive-Behavioral Therapy (CBT): Helps individuals identify and change thoughts and behaviors related to smoking.
- Motivational Interviewing: Enhances motivation to quit and develops a personalized quit plan.
- Group Therapy: Provides peer support and shared experiences in quitting.
Research has consistently shown that combining pharmacological treatments with behavioral therapy significantly improves quit rates compared to either approach alone13.
4. Digital Support Tools
In recent years, smartphone apps, text messaging programs, and online support groups have emerged as valuable tools in smoking cessation efforts. These digital interventions can provide real-time support, track progress, and offer personalized strategies for managing cravings and triggers.
Also Read:
What are Nicotine Salts?
Conclusion: Empowering Informed Choices for a Healthier Future
Nicotine, with its complex history and profound effects on human health, remains a significant public health challenge. However, advances in our understanding of nicotine addiction and the development of effective treatment strategies offer hope for those seeking to quit.
For individuals currently using nicotine products, it’s crucial to be aware of the risks and to consider the available options for quitting. Remember that quitting is a process, and it may take several attempts before achieving long-term success. Healthcare providers, support groups, and quit lines are valuable resources for anyone looking to break free from nicotine addiction.
For those who haven’t started using nicotine products, the best approach is prevention. Understanding the risks and addictive potential of nicotine can help individuals make informed decisions about their health.
As research continues and new technologies emerge, our approach to nicotine use and addiction will undoubtedly evolve. By staying informed and supporting evidence-based policies and interventions, we can work towards a future where the burden of nicotine addiction is significantly reduced.
References:
- Yerger, V. B., Przewoznik, J., & Malone, R. E. (2007). Racialized geography, corporate activity, and health disparities: tobacco industry targeting of inner cities. Journal of Health Care for the Poor and Underserved, 18(4 Suppl), 10-38. https://www.proquest.com/docview/220587746?sourcetype=Scholarly%20Journals ↩︎
- Centers for Disease Control and Prevention. (2020). Tobacco Product Use and Associated Factors Among Middle and High School Students — United States, 2019. MMWR Surveill Summ 2019;68(No. SS-12):1–22. https://www.cdc.gov/mmwr/volumes/68/ss/ss6812a1.htm ↩︎
- Benowitz, N. L. (2010). Nicotine addiction. New England Journal of Medicine, 362(24), 2295-2303.https://www.nejm.org/doi/full/10.1056/NEJMra0809890 ↩︎
- Benowitz, N. L., & Burbank, A. D. (2016). Cardiovascular toxicity of nicotine: Implications for electronic cigarette use. Trends in cardiovascular medicine, 26(6), 515-523. https://pubmed.ncbi.nlm.nih.gov/27079891/ ↩︎
- Ware, J. J., & Munafò, M. R. (2015). Genetics of smoking behaviour. Current topics in behavioral neurosciences, 23, 19-36.https://pubmed.ncbi.nlm.nih.gov/25655886/ ↩︎
- Gotts, J. E., Jordt, S. E., McConnell, R., & Tarran, R. (2019). What are the respiratory effects of e-cigarettes?. BMJ, 366, l5275.https://www.bmj.com/content/366/bmj.l5275 ↩︎
- Fluharty, M., Taylor, A. E., Grabski, M., & Munafò, M. R. (2017). The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine & Tobacco Research, 19(1), 3-13.https://pubmed.ncbi.nlm.nih.gov/27199385/ ↩︎
- Hajek, P., Phillips-Waller, A., Przulj, D., Pesola, F., Myers Smith, K., Bisal, N., … & McRobbie, H. J. (2019). A randomized trial of e-cigarettes versus nicotine-replacement therapy. New England Journal of Medicine, 380(7), 629-637. https://www.nejm.org/doi/full/10.1056/NEJMoa1808779 ↩︎
- Cullen, K. A., Gentzke, A. S., Sawdey, M. D., Chang, J. T., Anic, G. M., Wang, T. W., … & King, B. A. (2019). e-Cigarette use among youth in the United States, 2019. Jama, 322(21), 2095-2103. https://pubmed.ncbi.nlm.nih.gov/31688912/ ↩︎
- Layden, J. E., Ghinai, I., Pray, I., Kimball, A., Layer, M., Tenforde, M., … & Haupt, T. (2020). Pulmonary illness related to e-cigarette use in Illinois and Wisconsin—final report. New England Journal of Medicine, 382(10), 903-916. https://www.nejm.org/doi/full/10.1056/NEJMoa1911614 ↩︎
- Stead, L. F., Perera, R., Bullen, C., Mant, D., Hartmann‐Boyce, J., Cahill, K., & Lancaster, T. (2012). Nicotine replacement therapy for smoking cessation. Cochrane database of systematic reviews https://pubmed.ncbi.nlm.nih.gov/23152200/ ↩︎
- Cahill, K., Stevens, S., Perera, R., & Lancaster, T. (2013). Pharmacological interventions for smoking cessation: an overview and network meta‐analysis. Cochrane database of systematic reviews https://pubmed.ncbi.nlm.nih.gov/23728690/ ↩︎
- Stead, L. F., Koilpillai, P., Fanshawe, T. R., & Lancaster, T. (2016). Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database of Systematic Reviews https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD008286.pub3/full ↩︎
- Bestselling Vapes in UK After Disposable Ban: What to Stock 2025 - August 8, 2025
- Argentina Debates Stricter Vape Laws Amid Prohibition Failures - August 8, 2025
- Nigeria Advocacy Group Urged to Hike Tobacco & Vape Tax by 100% - August 8, 2025







